fascial adhesions
-
🤔 What Are Fascial Adhesions?
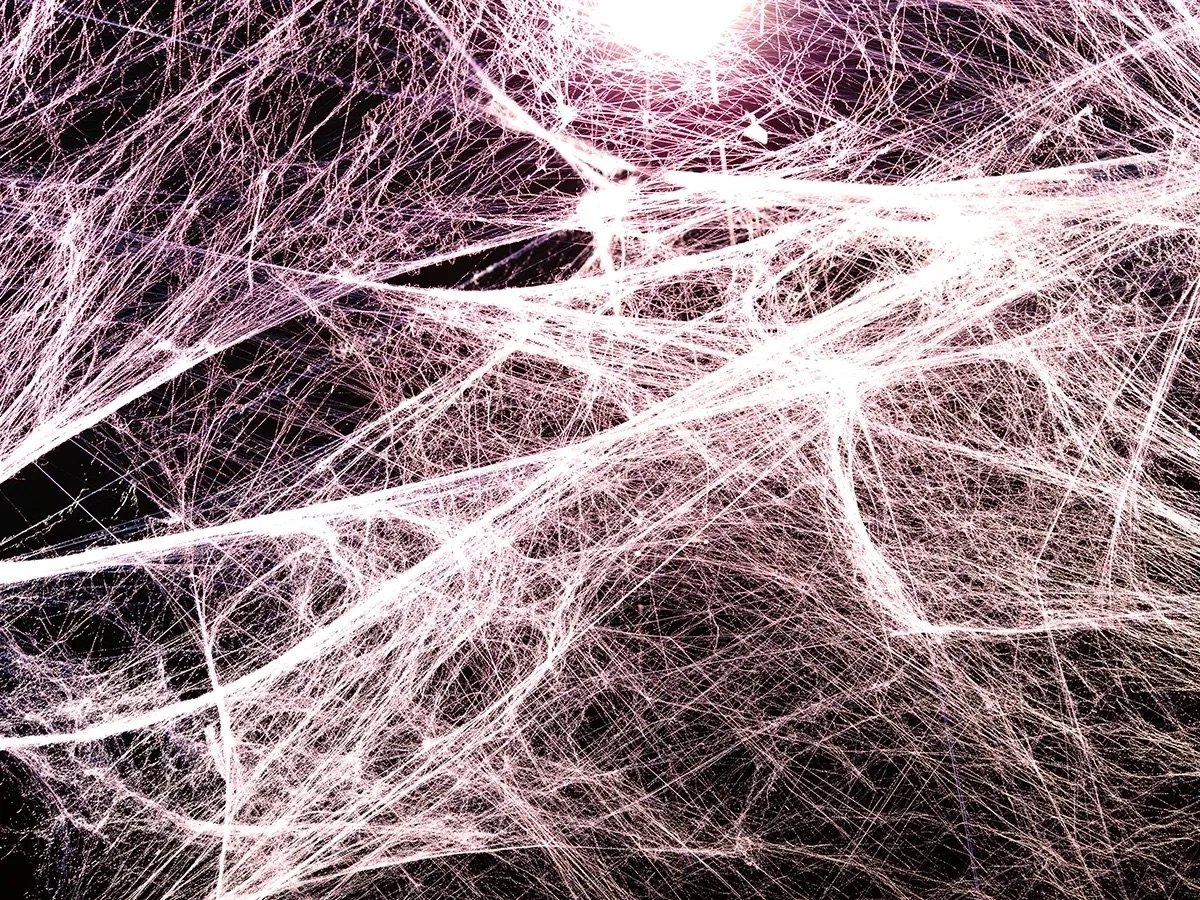
Fascia is a web-like tissue that connects every muscle, bone, nerve, and organ in the body. It allows everything to glide and move freely. But when fascia becomes stiff, stuck, or dehydrated, it creates adhesions — spots where tissues lose their glide and get ‘glued down.’
This can lead to:
Ongoing tightness or stiffness
A feeling of being “stuck” or “twisted”
Pain that doesn’t improve with stretching
Reduced movement, strength, or coordination
Referred pain to other areas
Fascial adhesions can develop from:
Injury or surgery
Overuse or repetitive movements
Poor posture
Inflammation or chronic illness
Immobilisation or scar tissue
🛠️ How Do We Treat It?
At Lowther Physiotherapy, we use a combination of:
Fascial scraping / IASTM (Instrument-Assisted Soft Tissue Mobilisation)
Dry needling to reduce local tissue tension
Myofascial release and cupping
Targeted movement retraining to restore full-body glide
Postural and strength rehab to prevent re-adhesion
🧭 Common Areas of Fascial Adhesion We Treat:
Thoracolumbar Fascia (Lower Back) – “band of tightness” across the back
Plantar Fascia (Feet) – morning tightness or pulling under the foot
Iliotibial Band (Outer Thigh) – stubborn tension that won’t release
Abdominal Wall & Diaphragm – rotation, breathing, and core dysfunction
Post-Surgical Scars – pulling or stiffness years after healing
Chest Wall & Pec Area – restriction with posture or overhead movement
Hip Flexors / Anterior Hip – deep groin tightness with lunging or running
Scapular Region – “sticky” shoulder blades or reduced overhead mobility
👩⚕️ How Physio Can Help:
Identify where your fascial system is restricted — even if it’s not where the pain is
Use hands-on and tool-assisted techniques to break up adhesions
Improve glide between tissue layers for smoother movement
Retrain your body to move efficiently again
Prevent re-adhesion through targeted strength and movement
🙋♀️ Answers to Common Questions
1. What does a fascial adhesion feel like?
Like a “knot” that doesn’t release
A dragging, pulling, or stuck sensation
Limited movement or tightness even without injury
Pain that moves or doesn’t match typical muscle patterns
2. Can you see adhesions on scans?
Not really — most fascial restrictions don’t show on X-rays or MRIs. But you’ll feel them, and physios can identify them through movement testing and palpation.3. Will stretching fix it?
Not often. Stretching only works if the tissues can glide. Adhesions need manual release and rehydration of the fascia.4. Is fascia work painful?
Sometimes it can be tender — especially if a restriction has been there a while. We’ll adjust intensity to your comfort level and combine it with movement-based recovery.5. How many sessions will I need?
It depends on how long the adhesions have been there, and what caused them. Some clients feel a difference in 1–2 sessions, while others benefit from a series of treatments with guided rehab.6. Will the adhesions come back?
Not if we correct the underlying movement issues and help you stay mobile, hydrated, and strong. That’s what our tailored rehab plan is for. -
🤔 What Is It?
The thoracolumbar fascia is a large sheet of connective tissue that spans your lower back and upper glute area, linking your spine, hips, ribs, and core. It acts like a central tensioning system for movement and stability.
When this fascia becomes restricted, stuck, or fibrotic, it can create:
A deep, vague "band of tightness" across the lower back
Pain that doesn’t respond to stretching or massage
Reduced rotation or extension through the spine
Difficulty with bending, squatting, or even breathing deeply
It’s often missed on scans and misunderstood as “just tight muscles” — but fascial restrictions can seriously affect load transfer, posture, and movement efficiency.
💡 What Causes It?
Repetitive bending, lifting, or poor lifting mechanics
Prolonged sitting or poor posture
Previous back injuries, even years ago
Scar tissue from spinal surgery or abdominal trauma
Chronic low back pain, even with “clear scans”
Dehydration or systemic inflammation
🛠️ What You Can Do:
✅ Use self-release tools like balls or scraping tools across the mid-back and lumbopelvic region
✅ Stay hydrated — fascia responds to water and movement
✅ Improve hip and core control to reduce tension across the fascia
✅ Avoid relying solely on stretching — adhesions need to be treated differently
✅ Get assessed for fascial mobility and loading strategies
👩⚕️ How Physio Can Help:
Identify restricted fascial planes using movement testing and palpation
Use scraping (IASTM), dry needling, cupping, or release techniques to restore glide
Re-educate movement through core bracing, breath control, and spinal mobility
Address compensations in glutes, hamstrings, or QL contributing to overload
Help reduce flare-ups with a structured rehab and mobility plan
🙋♀️ Answers to Common Questions
1. What does a thoracolumbar fascia adhesion feel like?
A band of tightness or pulling across your lower back
Restriction when you try to twist, hinge, or extend
Doesn’t ease with rest or basic stretching
Feels deep and stubborn, not like normal muscle soreness
2. Is it dangerous?
Not at all — but it can limit performance, mobility, and comfort. Left untreated, it often leads to compensation injuries elsewhere in the body.3. Can I stretch it out?
Not really — fascial adhesions need to be treated with hands-on therapy or specific release tools, then followed by movement retraining.4. Is this why my back always feels tight even if my scans are fine?
Possibly. Fascial dysfunction is a functional issue, not always a structural one — but it has a big impact on how your body moves and feels.5. What treatments work best?
Scraping / IASTM to break up restrictions
Dry needling or cupping for deeper tissue access
Myofascial release techniques and breath training
Core-focused movement retraining like dead bugs, bird-dogs, and DNS patterns
6. How long does it take to fix?
Some feel immediate relief after a session or two. More chronic cases may need 3–5 sessions plus dedicated home work to fully resolve and prevent recurrence. -
🤔 What Is It?
The plantar fascia is a thick band of connective tissue that runs from your heel to the base of your toes. It supports your arch, absorbs impact, and helps with propulsion during walking and running.
While most people have heard of plantar fasciitis, not all foot pain is inflammatory. Some cases involve fascial adhesions, where the plantar fascia becomes stuck or fibrotic, limiting foot mobility and altering the way your foot loads.
You might notice:
A pulling, tugging, or stuck feeling under your foot
Pain when stretching your toes or walking barefoot on hard floors
Tightness that returns daily, especially in the morning
A sensation like the foot won’t roll smoothly when walking
💡 What Causes It?
Chronic overuse from walking, running, or standing on hard surfaces
Poor arch control or collapsing feet (overpronation)
History of plantar fasciitis that never fully resolved
Walking barefoot for long periods or wearing unsupportive shoes
Post-surgical scarring or tension in the foot and calf complex
🛠️ What You Can Do:
✅ Use a massage ball or scraping tool to mobilise the fascia (focus on heel to forefoot glide)
✅ Wear supportive footwear around the house to avoid repeated irritation
✅ Strengthen foot muscles — especially the intrinsics and tibialis posterior
✅ Mobilise the calf and big toe joints, which often restrict fascia movement
✅ Get assessed for foot mechanics and compensations
👩⚕️ How Physio Can Help:
Confirm whether your pain is fascial, neural, or joint-based
Use scraping, dry needling, cupping, or taping to reduce fascial tension
Teach you how to load and strengthen the arch properly
Address contributing factors like hip strength or poor foot posture
Guide return to walking or running without flare-ups
🙋♀️ Answers to Common Questions
1. What does plantar fascia adhesion feel like?
A tight band or tug under your foot, especially in the morning
Doesn’t fully respond to stretching or rolling
Pain with walking barefoot or standing too long
May feel like “the tissue’s stuck” when you bend your toes
2. Is this the same as plantar fasciitis?
Not quite — fasciitis is inflammatory, whereas adhesion is mechanical. Both can cause pain, but treatment differs: adhesions need mobility and glide restoration.3. Can I run with it?
Sometimes — but you’ll need to manage load carefully and restore foot mobility. Running with stiff fascia can overload other structures (Achilles, knee, hip).4. Will orthotics fix this?
Orthotics may help short-term by offloading the fascia, but lasting change comes from manual therapy + foot strength and mobility work.5. What treatments work best?
Scraping / IASTM under the arch and heel
Ball or bottle rolling + toe extension holds
Short foot, toe yoga, and calf-arch connection drills
Strengthening of tibialis posterior, glutes, and single-leg balance
6. How long does it take to improve?
You may feel relief within 1–3 sessions, but lasting changes typically require 4–6 weeks of combined treatment and home strength work. -
🤔 What Is It?
The iliotibial band (ITB) is a thick band of fascia running down the outside of your thigh, from the hip to just below the knee. It helps stabilise the leg during walking, running, and squatting — but it’s not a muscle and doesn’t “stretch” like one.
Instead of being tight, many people experience fascial adhesion or restriction in the ITB and its surrounding lateral line. This limits tissue glide and alters how load moves through the hip and knee.
You might feel:
A deep, persistent tightness down the outside of the thigh
Discomfort or pulling with squatting, lunging, or running
Outer knee irritation (often mistaken for ITB syndrome)
Relief that’s short-lived after foam rolling
💡 What Causes It?
Repetitive load from running, jumping, or squatting
Poor hip control or glute weakness
Over-reliance on the ITB for leg stability
Adhesions between the ITB and vastus lateralis or lateral quads
Scar tissue or strain post-injury or surgery
🛠️ What You Can Do:
✅ Avoid excessive foam rolling — focus instead on targeted release work
✅ Strengthen glutes and improve hip-pelvis control
✅ Mobilise the fascia using scraping or ball work near the hip and lateral knee
✅ Train posterior chain dominance (glutes and hamstrings)
✅ Get assessed for full kinetic chain loading patterns
👩⚕️ How Physio Can Help:
Identify whether your tightness is muscular, fascial, or neural
Apply scraping (IASTM), cupping, or dry needling along the lateral line
Release restrictions between the ITB and adjacent muscles
Train glute function and single-leg load tolerance
Help you move better without depending on the ITB for stability
🙋♀️ Answers to Common Questions
1. Why does my ITB always feel tight?
Because it likely has adhesions, not tight muscle tissue. The ITB itself doesn’t contract — but tension and lack of glide can make it feel tight.2. Should I foam roll it?
Rolling can help short term, but it doesn’t break up adhesions. Focus on deep tissue mobilisation and strength retraining for longer-lasting results.3. What’s the difference between ITB syndrome and adhesions?
ITB syndrome causes inflammation and pain at the knee, while adhesions create tightness or movement restriction along the whole band — often higher up near the hip.4. What treatments work best?
IASTM / scraping, dry needling to glute-ITB interface
Glute medius, glute max, and hamstring activation
Lateral chain mobility drills (e.g. lateral lunges, side planks)
Pelvis and core retraining for stability
5. Can I keep training?
Yes — but with modified loading and better movement patterns. Avoid training through high irritation and focus on activation + control.6. How long does it take to resolve?
Usually 1–4 sessions plus a few weeks of consistent home rehab will significantly improve glide and function. -
🤔 What Is It?
The front of the hip — especially the area around the iliopsoas, rectus femoris, and anterior hip capsule — is one of the most common sites of fascial restriction.
This area links the spine, pelvis, and thigh, and needs to move freely during walking, squatting, running, and lunging. When fascial tissues here become stuck, fibrotic, or adhered, you may feel:
A pinching or gripping sensation at the front of the hip
Inability to fully extend the hip — especially noticeable when walking or sprinting
Pain with lunges, step-ups, or lying flat
Tightness that doesn’t respond to stretching
💡 What Causes It?
Sitting for long periods with hips in a flexed position
Previous hip or groin injuries
Poor hip extension mechanics during walking or training
Adhesions between the psoas, iliacus, and surrounding fascia
Scar tissue or post-surgical fibrosis (e.g. hip arthroscopy)
🛠️ What You Can Do:
✅ Mobilise the anterior hip with release balls, hip flossing, and breathwork
✅ Train hip extension through glute and hamstring activation
✅ Avoid aggressive stretching — adhesions need release, not just lengthening
✅ Include pelvis and trunk control exercises
✅ Get physio assessment for hip glide, capsule mobility, and fascial tension
👩⚕️ How Physio Can Help:
Identify whether your restriction is muscular, capsular, or fascial
Use scraping, dry needling, cupping, or fascial release to restore tissue glide
Rebuild proper hip extension with glute reactivation and trunk integration
Address postural factors or gait faults contributing to the overload
Prevent recurrence through targeted movement retraining
🙋♀️ Answers to Common Questions
1. What does anterior hip adhesion feel like?
A deep tightness or pinching at the front of the hip
Feels “stuck” when lunging or stretching
May limit stride length or feel like the leg can’t fully extend
Often mistaken for hip flexor strain
2. Can you stretch it out?
Not effectively — adhesions restrict glide between tissue layers, not just muscle length. You need manual therapy + movement retraining.3. Is this why I can’t lunge or run properly?
Quite possibly. Limited hip extension from adhesions affects stride, glute activation, and spinal mechanics — which can cause knock-on effects.4. What’s the difference between a tight muscle and a fascial adhesion?
Tight muscles respond to stretching and rest. Adhesions feel like a deep pull or block and need to be manually released.5. What treatments work best?
IASTM or dry needling to the iliacus, psoas, and anterior capsule
Glute bridges, split stance work, and DNS patterns
Active hip mobility drills like 90/90 transitions and kneeling hip openers
Core and pelvic positioning retraining
6. How long does it take to resolve?
Some cases respond in just 1–2 sessions, while chronic or post-surgical restrictions may require 6+ sessions plus 4–6 weeks of rehab. -
🤔 What Is It?
The scapula (shoulder blade) is designed to glide smoothly over the rib cage during arm and shoulder movement. It connects to the body through a network of fascia, muscles, and nerve-rich soft tissues.
When these tissues become adhered or restricted, especially between the subscapularis, serratus anterior, and thoracic fascia, the scapula can feel:
“Stuck” or “grinding” when moving
Limited in reaching, lifting, or overhead motion
Associated with upper back tightness or neck tension
Weak or unstable during pushing or pulling movements
💡 What Causes It?
Poor posture or prolonged shoulder rounding
Repetitive overhead lifting or loading
Previous shoulder injuries or rotator cuff dysfunction
Lack of thoracic mobility or rib cage stiffness
Scapulothoracic fascial adhesions or capsular tightness
🛠️ What You Can Do:
✅ Mobilise the scapula and thoracic fascia using ball release or cupping
✅ Improve mid-back mobility to allow scapular freedom
✅ Strengthen scapular stabilisers like serratus anterior and lower traps
✅ Incorporate breathwork and posture resets
✅ Get physio assessment to rule out joint or nerve restrictions
👩⚕️ How Physio Can Help:
Assess scapular rhythm and fascial glide
Apply IASTM, cupping, or dry needling to improve scapulothoracic mobility
Retrain scapular movement through closed-chain and wall drills
Integrate thoracic spine mobility to enhance shoulder mechanics
Build strength in rotator cuff and postural control systems
🙋♀️ Answers to Common Questions
1. What does a scapular adhesion feel like?
A sense that the shoulder blade doesn’t move freely
Stiffness or ache with overhead or reaching motions
Localised or referred pain into the neck, shoulder, or upper back
Clicking or grinding sensation during movement
2. Can I stretch it out?
Stretching alone rarely helps — fascial adhesions need hands-on or tool-assisted mobilisation, followed by retraining scapular control.3. Is this causing my shoulder pain?
Possibly. Scapular dysfunction contributes to impingement, tendinopathy, and instability — and adhesions are often the root.4. What treatments work best?
Scraping or cupping under the scapula (subscapularis, serratus)
Wall slides, serratus punches, thoracic extension drills
Quadruped and side-lying scapula drills to restore rhythm
Breath and rib cage work for trunk-scapula coordination
5. How long will it take to improve?
Mild cases: 1–3 sessions + home drills
More chronic dysfunction: 2–5 sessions & 4+ weeks of retraining -
🤔 What Is It?
The chest wall — especially the pectoralis major and minor, upper ribs, and anterior shoulder fascia — plays a key role in posture, shoulder movement, and breath control.
When the fascia in this area becomes tight, thickened, or adhered, it limits how the shoulders open and affects the shoulder, neck, and even breathing.
You may feel:
A sensation of tightness or compression across the front of the chest
Restricted overhead or reaching movement
Postural fatigue, neck tightness, or poor scapular control
Difficulty with deep breathing, especially under load or stress
💡 What Causes It?
Prolonged forward posture, especially at desks or driving
Upper body weight training without proper mobility
Repetitive reaching, pressing, or poor push-up mechanics
Post-surgical or scar-related fascial thickening (e.g. breast surgery, pacemaker)
Chronic stress breathing patterns or rib stiffness
🛠️ What You Can Do:
✅ Use a trigger ball, scraping, or cupping across the pecs and ribs
✅ Strengthen posterior chain muscles (mid-back, rotator cuff, traps)
✅ Improve thoracic mobility and breathing patterns
✅ Perform pec lengthening drills with neural control
✅ Get physio support to assess scapular and trunk loading
👩⚕️ How Physio Can Help:
Release adhesions through manual therapy, dry needling, or fascial scraping
Improve shoulder mechanics with thoracic and scapular mobility drills
Retrain posture and breath using diaphragmatic and DNS-style techniques
Support your return to full range and control — without re-tightening
Address related issues like shoulder impingement, neck strain, or tension headaches
🙋♀️ Answers to Common Questions
1. What does chest wall adhesion feel like?
A tight, restricted, or compressed sensation across the front of the chest
Limited range with overhead motion or backward reaching
Pulling across the pec when stretching or opening up
Postural fatigue or shoulder instability
2. Is this from my posture?
Quite possibly. Sitting for long hours encourages fascial stiffening in the pecs and anterior shoulder. It builds over time unless treated and reversed.3. Can I just stretch it out?
Stretching may help temporarily — but fascial adhesions need hands-on or tool-assisted release to create lasting glide.4. Can this cause shoulder or neck pain?
Yes. Pec tightness limits scapular motion and contributes to impingement, headaches, or nerve compression (especially with tight pec minor).5. What treatments work best?
Scraping, dry needling, and cupping over pec major and minor
Wall angels, doorway openers, and thoracic extension drills
Scapular retraction work (rows, YTWs)
Breath and rib cage mobility for long-term postural reset
6. How long does it take to resolve?
Most people feel relief within 1–3 sessions, but full postural and movement change may take 4–6 weeks of consistent rehab and control work. -
🤔 What Is It?
Your abdominal fascia and diaphragm are central to nearly every movement and function in your body — from core control and posture to breathing, digestion, and spinal mobility.
When the fascia here becomes stuck, dehydrated, or adhered (often after surgery, trauma, or inflammation), it can limit:
Torso rotation and side bending
Full breathing capacity
Core activation and spinal stability
Hip and rib cage movement
Even contribute to gut symptoms or pelvic tension
You may feel:
A stiff, locked feeling through the front of the core
Pain with twisting, rolling, or arching your back
Limited breath depth, often worse with stress
Pulling or discomfort around scars or the belly
“Disconnected” from your core despite training
💡 What Causes It?
Abdominal surgery (C-section, hernia, appendix, laparoscopy, endometriosis procedures)
Chronic gut inflammation or bloating
Postural or breathing dysfunction
Core bracing or tension under stress (especially in athletes)
Adhesions between organs, fascia, and muscle layers
🛠️ What You Can Do:
✅ Begin gentle belly and diaphragmatic breathwork
✅ Use cupping, fascial scraping, or ball release over the abdominals
✅ Train rotational mobility (e.g. open books, 90/90 transitions)
✅ Rebuild proper intra-abdominal pressure with core coordination drills
✅ Get assessed for scar restrictions or movement limitations
👩⚕️ How Physio Can Help:
Identify fascial restrictions using palpation, breath testing, and movement patterns
Release adhesions with visceral mobilisation, scraping, dry needling, or cupping
Guide breath mechanics with diaphragm-focused rehab
Reintegrate the core with DNS-style bracing, rotation, and load sharing
Address secondary issues like hip mobility, back pain, or pelvic tension
🙋♀️ Answers to Common Questions
1. What does abdominal adhesion feel like?
A feeling of being stiff, blocked, or unable to twist or breathe fully
Pulling around scars, the belly, or even the ribs
Pain or restriction when lying flat or doing core exercises
Poor connection to deep core muscles, despite training
2. Can this affect my breathing?
Yes — fascial restriction around the diaphragm, ribs, or abdominal wall can limit expansion and contribute to shallow, stress-driven breathing.3. Is this from my C-section or abdominal surgery?
Highly likely. Scar tissue often causes fascial restriction that can spread through the trunk and affect movement long after the incision has healed.4. Can it affect digestion or gut issues?
Yes — fascial stiffness can impair visceral movement, reduce abdominal tone, and contribute to bloating, reflux, or constipation in some cases.5. What treatments work best?
Manual therapy, cupping, and scraping over the belly and ribs
Diaphragmatic breathwork and core re-coordination
Thoracic and hip mobility drills to restore global movement
Scar release techniques for surgical adhesions
6. How long to see change?
Some clients feel immediate lightness or breath improvement after 1–2 sessions. More chronic post-surgical or gut-related cases may need 4–8+ sessions plus home practice. -
🤔 What Is It?
After surgery, the body naturally forms scar tissue to heal the area. But sometimes, that scar tissue creates adhesions — thickened, fibrous bands that stick to surrounding fascia, muscle, or organs.
These adhesions can:
Restrict movement and mobility, even in distant areas
Cause pulling, pinching, or tightness around the scar
Alter how muscles activate or load
Create pain or stiffness years after the surgery has healed
You might notice:
Difficulty stretching, twisting, or loading near the scar
Sensitivity or tension when pressing near the area
Reduced strength or coordination on the affected side
Pain in seemingly unrelated areas due to compensations
💡 What Causes It?
Any surgical procedure:
C-sections, hernia repair, hip/knee replacements, spinal surgery, ACL recon, abdominal laparoscopy, etc.
Immobilisation or lack of post-op rehab
Scar tissue forming in areas with high movement or fascial cross-links
Pre-existing postural issues or fascial stiffness
🛠️ What You Can Do:
✅ Gently mobilise the scar with cupping, scar massage, or scraping tools
✅ Restore movement with mobility and rotation drills
✅ Strengthen surrounding areas to restore function
✅ Avoid ignoring the scar — it can impact your whole kinetic chain
✅ See a physio trained in fascial and post-surgical recovery
👩⚕️ How Physio Can Help:
Assess the mobility, texture, and reactivity of scar tissue
Use tools like IASTM (scraping), dry needling, cupping, or manual release
Integrate scar release into your whole-body rehab plan
Improve muscle activation, joint control, and movement quality
Help prevent recurrence of compensatory pain or stiffness
🙋♀️ Answers to Common Questions
1. Can scar tissue cause pain years after surgery?
Yes — adhesions can create pulling, tension, and altered load long after the wound has healed, especially if they limit glide between layers.2. Why does my scar feel tight or stuck?
Because the fascia beneath the skin may be bound down, restricting the normal movement between muscles, nerves, and skin layers.3. What if my scar looks healed on the outside?
Even if it looks fine, internal adhesions can limit movement or cause dysfunction. They’re functional, not always visible.4. Can physio actually fix this?
Yes — we can release the fascia, retrain movement, and reduce symptoms with a combination of manual therapy and corrective rehab.5. What treatments help post-surgical scars?
Cupping and scraping over and around the scar
Manual therapy and massage to improve tissue glide
Scar mobility drills and load retraining
Whole-body movement integration (especially with spinal or abdominal surgeries)
6. How long does it take to improve?
Some people feel changes after just 1–2 sessions, while more complex cases may take longer.
